The bacterium produces a particular protein that allows it to sneak past the human immune system even while triggering inflammation.
ABOVE:© ISTOCK.COM, LUISMMOLINA
EDITOR’S CHOICE IN IMMUNOLOGY
Jörn Coers, an immunologist at Duke University, says the world is facing a silent pandemic: chlamydia. The US Centers for Disease Control and Prevention (CDC) estimates that 4 million people contracted the bacterial disease in 2018, making it the most commonly diagnosed sexually transmitted infection. Even so, most infections go undiagnosed, he says, and infections can persist for months. Chlamydia infections cause inflammation, which can lead to fibrosis in the reproductive tract. In men, symptoms are generally mild, but women face a risk of ectopic pregnancies and infertility.
In an effort to speed up chlamydia vaccine development, Coers has spent years figuring out how Chlamydia trachomatis, the causative bacterium in humans, evades destruction. In a recent study, Coers and his team discovered a key protein that allows C. trachomatis to slip past the body’s defenses.
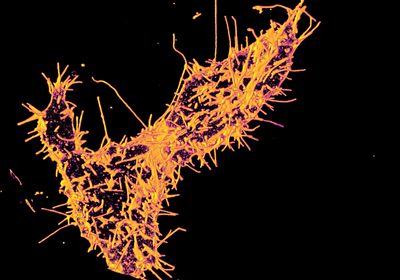
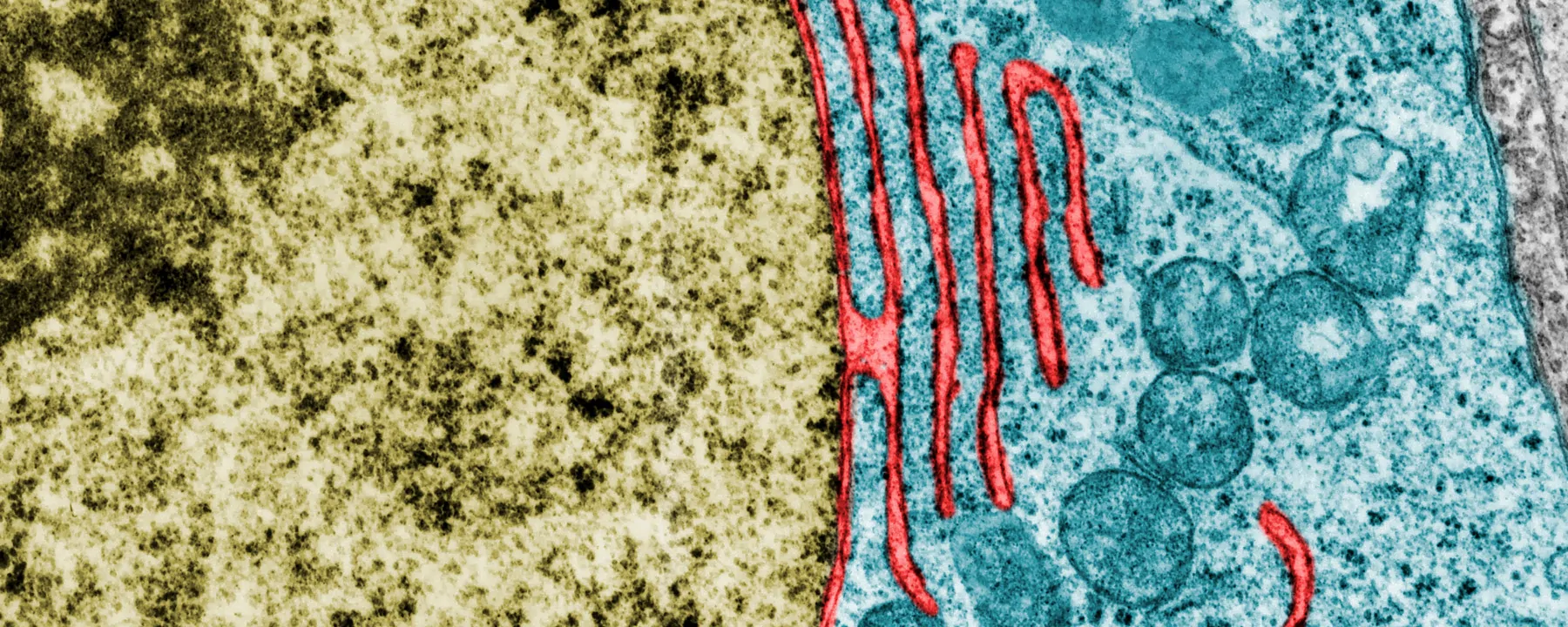
To enter a host cell, Chlamydia cloaks itself in a piece of the host cell’s membrane, forming a vacuole, or inclusion, where it grows and divides uninterrupted by immune cells. T cells can detect Chlamydia in the brief time it lives outside the cell and, in response, release gamma interferon (IFN-γ), an inflammatory cytokine that triggers destruction of the pathogen. But something about the inclusion allows Chlamydia to hide from the immune response and persist for months or years.
Several years ago, Coers and his colleagues noticed that C. trachomatis excels at evading the human immune system while C. muridarum, a closely related rodent pathogen, doesn’t. In a 2016 study, Coers discovered that the protein ubiquitin binds to C. muridarum inclusions in human cells and targets them for destruction, but something about C. trachomatis inclusions lets them avoid ubiquitin binding. In the new study, the researchers sought to understand how.
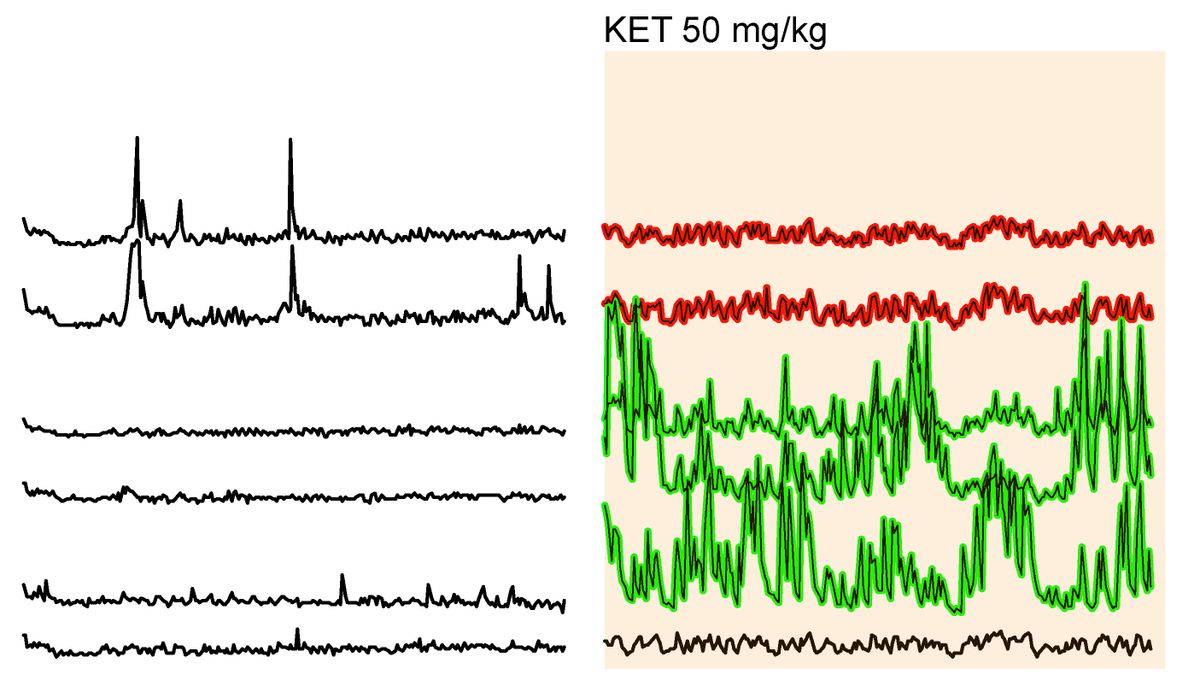
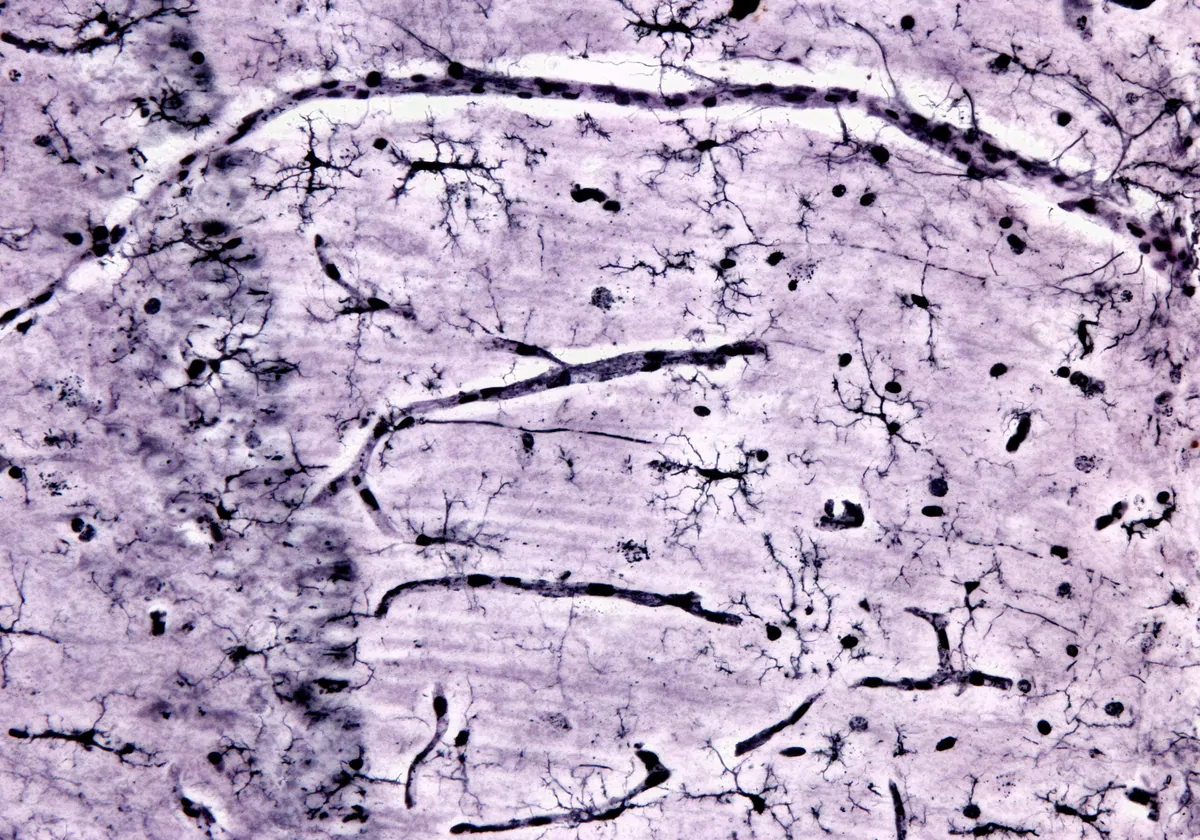
Chlamydia invades a host cell, forms a membrane-bound vacuole, or inclusion, and then modifies the protein composition of the structure’s membrane. If immune cells detect Chlamydia before it forms the inclusion, they trigger T cells to produce interferon-γ (IFN-γ), a powerful cytokine. IFN-γ activates the protein mysterin (also called RFN213), which attaches ubiquitin to the inclusion membrane, signaling the cell to destroy the inclusion’s contents by dumping them into a lysosome (left). C. trachomatis produces GarD, a protein that integrates into the inclusion membrane itself and somehow prevents mysterin from attaching ubiquitin, allowing the bacterium to evade immune destruction while continuing to multiply and eventually bursting from the cell (right). WEB | PDF
© NANOCLUSTERING.COM
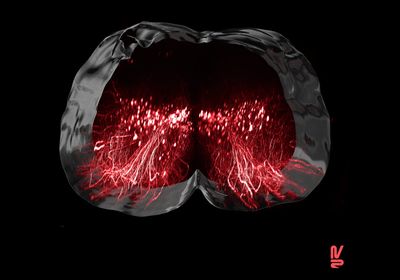
The team performed a genetic screen of various mutated C. trachomatis strains grown inside human epithelial cells in the presence and absence of IFN-γ. The C. trachomatis strains most susceptible to IFN-γ-mediated destruction had mutations in a gene that encodes a protein the researchers named GarD (formerly CTL0390), indicating that GarD is important for C. trachomatis’s survival. Imaging experiments on IFN-γ-resistant C. trachomatis strains revealed that GarD blocks ubiquitin binding by inserting itself into the inclusion membrane. Disabling GarD allowed ubiquitin binding and left the bacteria vulnerable. Meanwhile, mice defend themselves from rodent-infecting C. muridarum by blocking ubiquitin via a different mechanism entirely.
I think it’s an important and reliable result. It shows just how evasive Chlamydia is.
—Bob Brunham, University of British Columbia
“When the GarD protein is there, the inclusion . . . disguises itself, like an invisibility cloak from Harry Potter,” Coers explains. “Now we understand why interferon-γ is not able to clear infections and why these infections last for such a long time.”
“I think it’s an important and reliable result,” says Bob Brunham, an infectious disease scientist and professor emeritus at the University of British Columbia who was not involved in the study. “It shows just how evasive Chlamydia is.”
The researchers also discovered that IFN-γ activates a protein called mysterin (also called RNF213) that’s responsible for attaching ubiquitin to the inclusion, though Coers notes that how exactly GarD prevents mysterin from doing so remains, aptly, a mystery.