The biotech company Verve Therapeutics launched the study with the aim of using base editing to treat a genetic condition that causes high cholesterol and increases a person’s risk of developing cardiovascular disease.
ABOVE:© ISTOCK.COM, VCHAL
Update (November 7): The US Food and Drug Administration (FDA) today announced a hold on Verve Therapeutics’s Investigational New Drug (IND) application, according to a press release. The federal agency will be sending a list of questions within 30 days, and Verve “intends to work closely with the FDA to resolve the hold as promptly as possible in order to initiate dosing in the U.S.” The company recently completed a first round of dosing in three patients in New Zealand and the UK, and reported no drug-related adverse effects. An independent Data Safety Monitoring Board reviewed safety data from the first cohort and recommended that the trial proceed to a second, higher dosage.
Verve Therapeutics announced today (July 12) that it has dosed the first participant in a clinical trial assessing the safety and tolerability of the gene editing platform VERVE-101, which uses a precise kind of gene editing called base editing. By changing a single DNA nucleotide, VERVE-101 can inactivate a gene expressed in the liver that is linked to high cholesterol in people with a hereditary and potentially life-threatening subtype of cardiovascular disease called heterozygous familial hypercholesterolemia (HeFH).
“The dosing of the first human with such an investigational base editing medicine represents a significant achievement by our team and for the field of gene editing,” Sekar Kathiresan, the cofounder and chief executive officer of Verve Therapeutics, says in a press release. “Preclinical data suggest that VERVE-101 has the potential to offer people with HeFH a game-changing treatment option, transforming the traditional chronic care model to a single-course, life-long treatment solution.”
Prior to the trial, HeFH and other conditions that manifest in high levels of LDL cholesterol (so-called bad cholesterol) were treated using dietary and lifestyle changes combined with cholesterol-lowering drugs that have to be administered one or two times a month. This regimen can be difficult for patients to adhere to, Gary Balady, the director of preventive cardiology at Boston Medical Center, tells The Boston Globe, and only about 20 percent of patients are able to achieve their goals. Balady, who was not involved in the trial, adds that “having a one-time treatment has the potential to save lots of lives.”
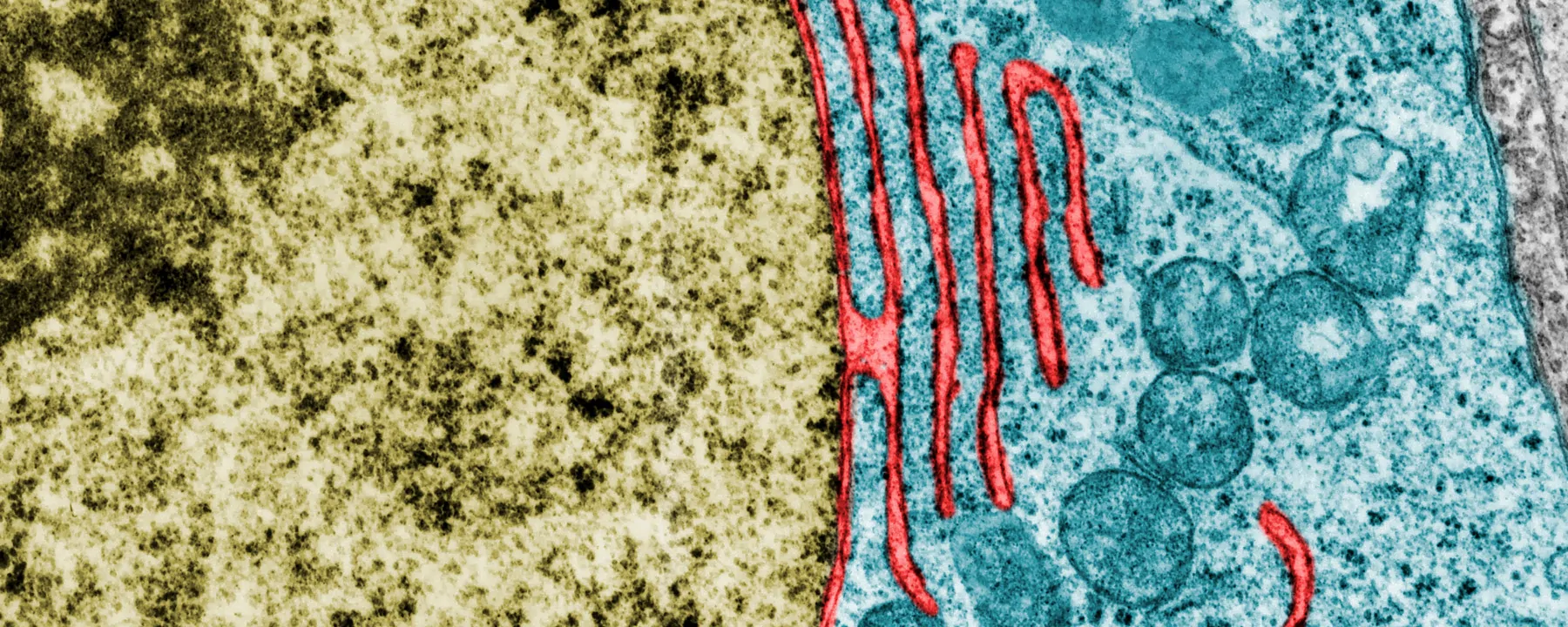
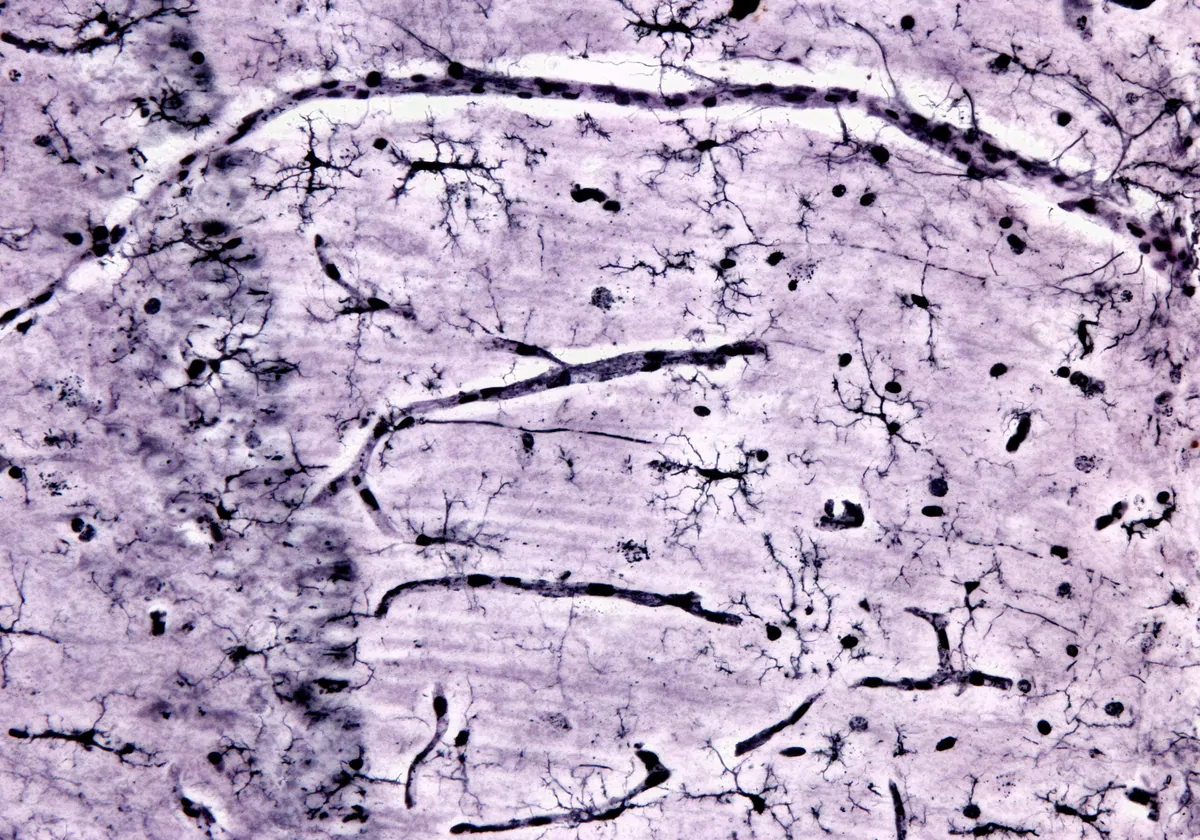
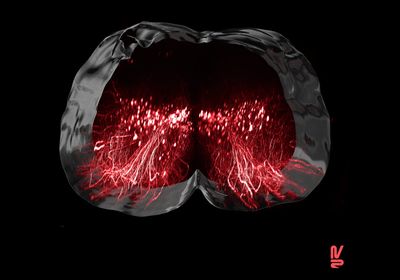
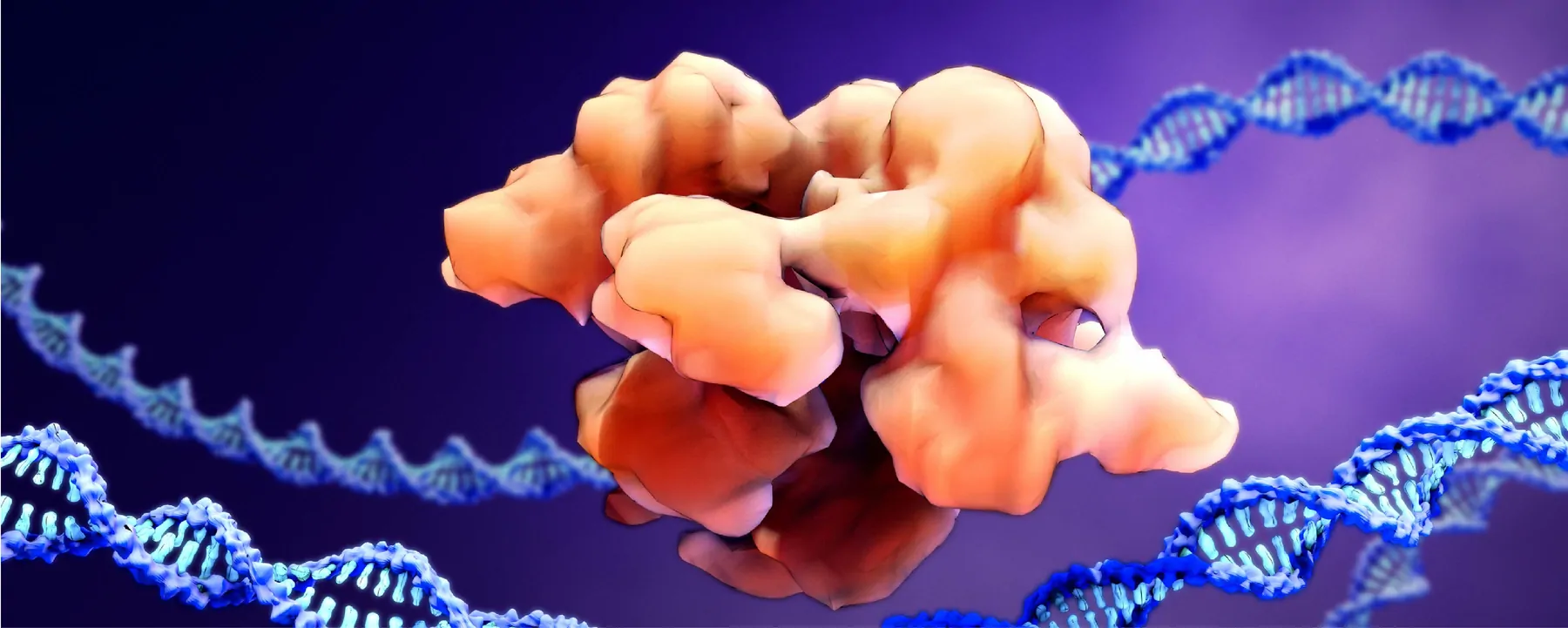
VERVE-101 edits a single nucleotide within the genetic code for PCSK9, a gene expressed in the liver. PCSK9 encodes an enzyme that regulates the amount of cholesterol in the plasma by binding to LDL receptors on liver cell membranes. Certain heritable forms of HeFH are caused by mutations in the genes; by substituting an adenine base for a guanine, the base editing tool induces a new, intentional mutation that renders the defective gene inactive, lowering the level of LDL in a person’s body and, consequently, reducing the risk of developing cardiovascular diseases such as HeFH.
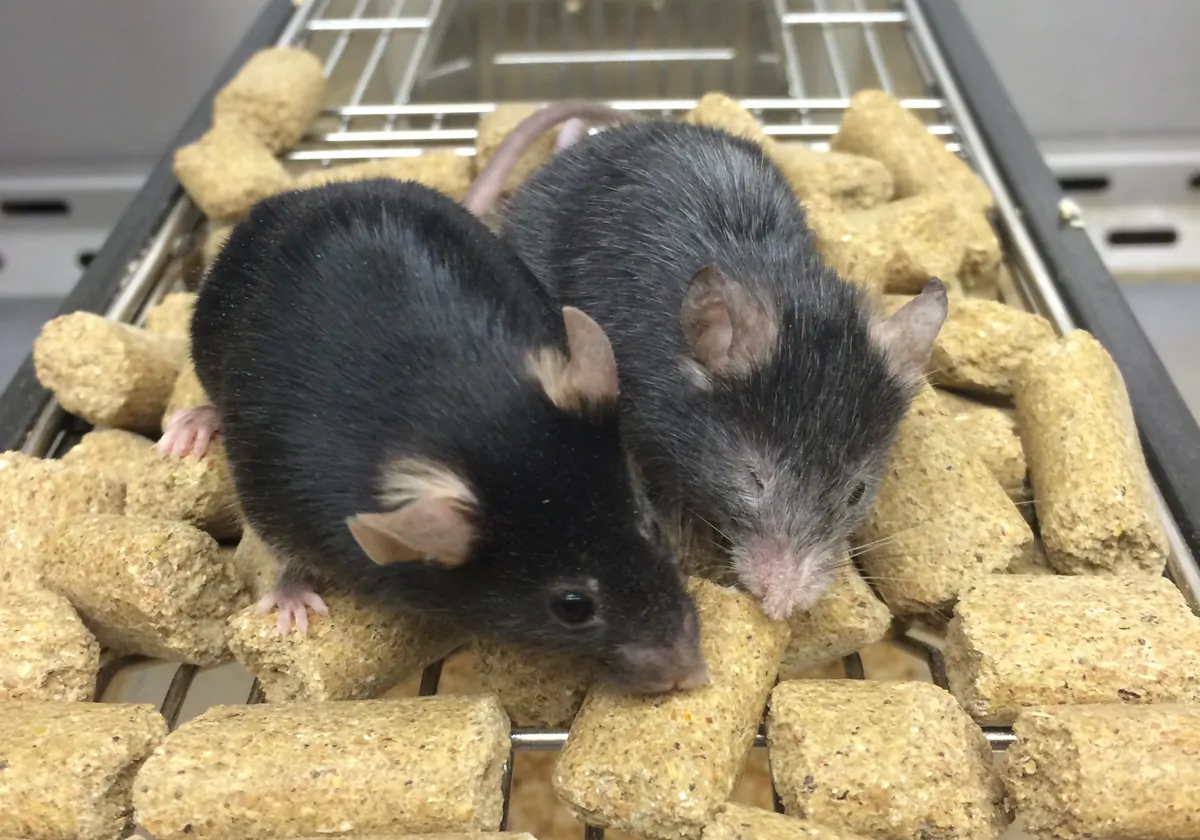
In preclinical studies using nonhuman primates, VERVE-101 lowered levels of LDL cholesterol by roughly 70 percent after two weeks, and the levels remained low for at least two years, Kathiresan tells the Globe.
“This seems like a bigger effect than I would have predicted,” Sarah de Ferranti, the chief of ambulatory cardiology at Boston Children’s Hospital, who was not involved in the work, tells the Globe. She adds that even if the treatment were only half as effective in humans, “I still think that would be a huge game changer.”
The human trial, which received regulatory approval in May, includes roughly 40 adults with HeFH who will receive one of three dosing regimens. The first person to receive a dose lives in New Zealand, where the trial was approved, but Verve Therapeutics also plans to seek permission from regulators this year to expand it into the UK and the US, Biopharma Dive reports. Preliminary trial results are expected in 2023.
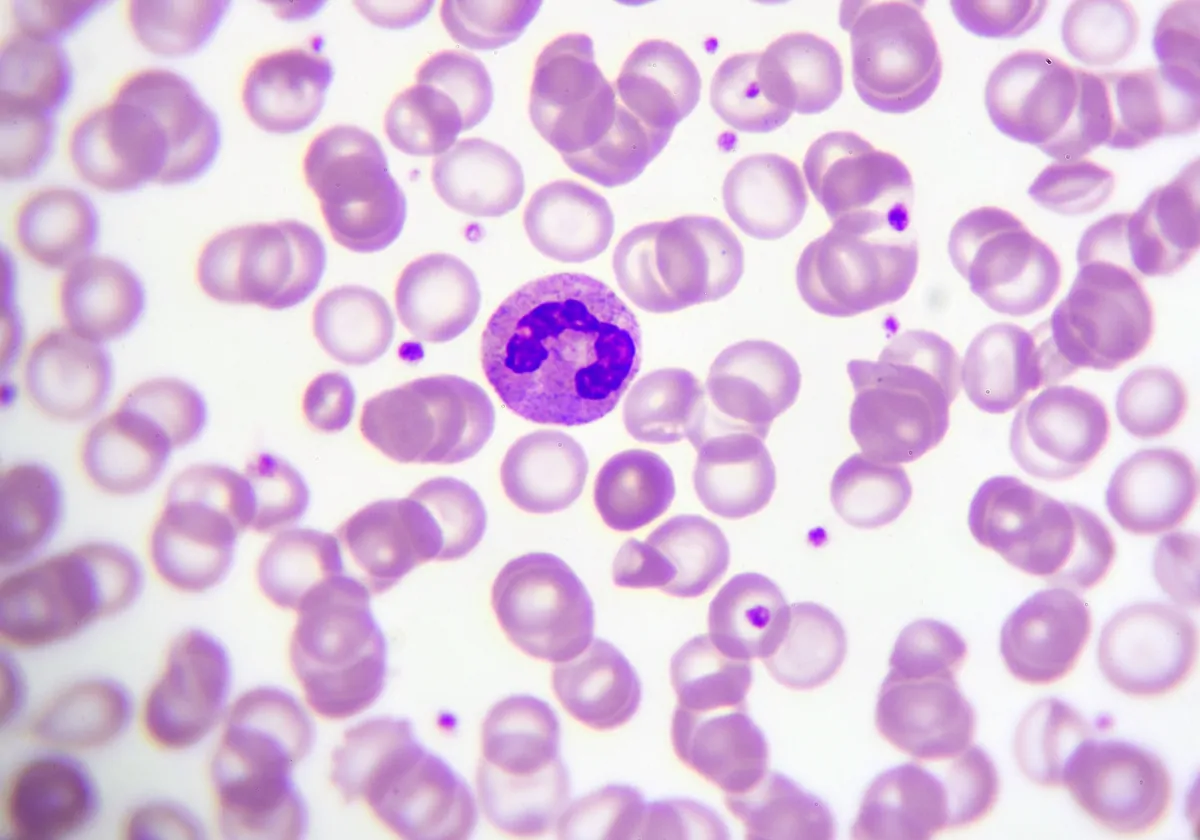
Base editing technology has only recently made its way to human trials, and VERVE-101 is not the first. This year, researchers at University College London launched a clinical trial to treat leukemia using base editing tools, and the Boston-based biotech company Beam Therapeutics, which licensed some of its technology to Verve Therapeutics, will launch a trial later this year using a base editor to treat people with blood disorders such as sickle cell disease and beta thalassemia, the Globe reports. But these trials involve modifying patients’ cells outside of their body before infusing them back in; Verve Therapeutics joins a short list of companies that have developed treatments meant to edit genes directly in the body.
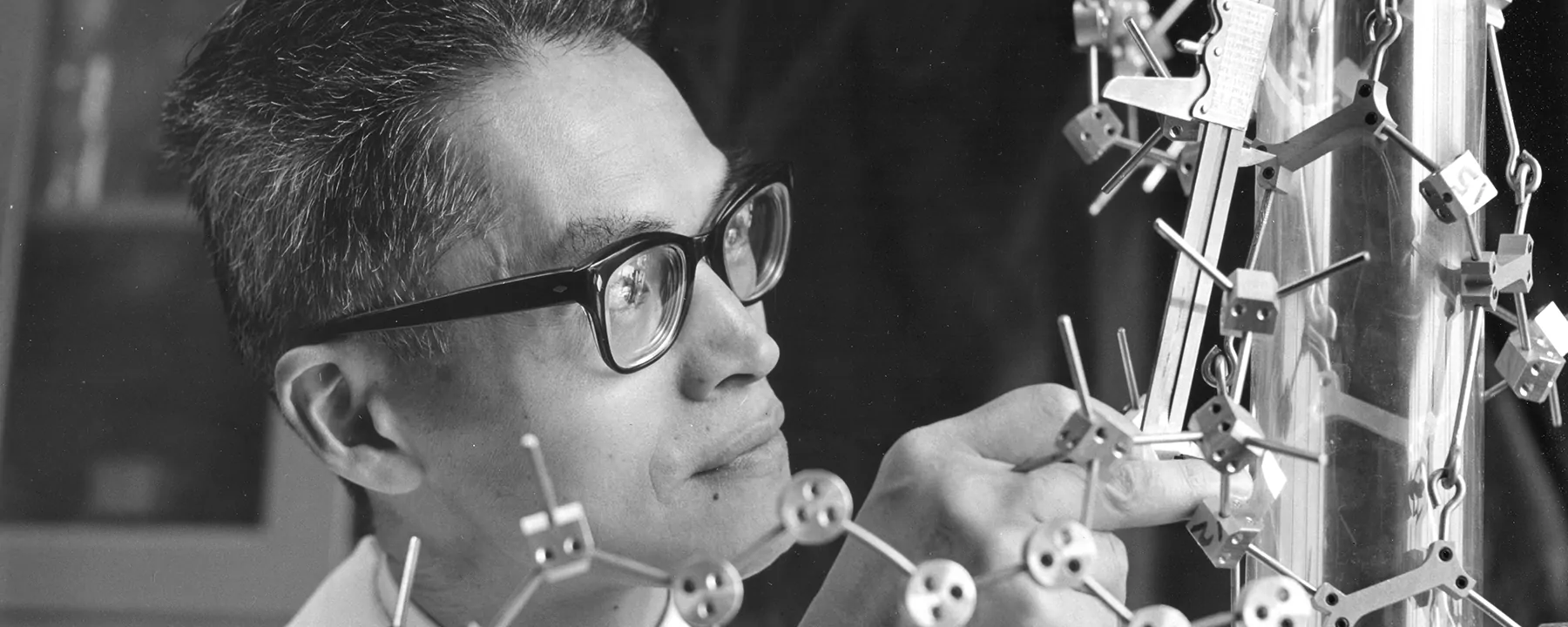
David Liu, the Broad Institute of MIT and Harvard University researcher who first developed base editing in 2016, tells the Globe that he hopes to see many more platforms in the coming year, noting that “to be able to take control of our genomes, to me, is one of the most human things we can do” to alleviate suffering.
But Jennifer Doudna of the University of California, Berkeley, one of the researchers credited with coinventing CRISPR gene editing in 2012, notes that even base editing—generally thought to be safer than other CRISPR techniques because it manipulates a smaller chunk of the genome—is not without risk, and she doesn’t yet think CRISPR has the precision to correct point mutations. There can be off-target effects, she tells the Globe, meaning that you “end up usually getting more editing than you might want.”
See “Base Editors Cause Off-Target Mutations in RNA”
The repercussions of these effects are not yet known, but John Evans, the chief executive of Beam Therapeutics, tells the Globe that these off-target edits are somewhat predictable, and potentially something that can be avoided. “You can kind of engineer around it,” he says.