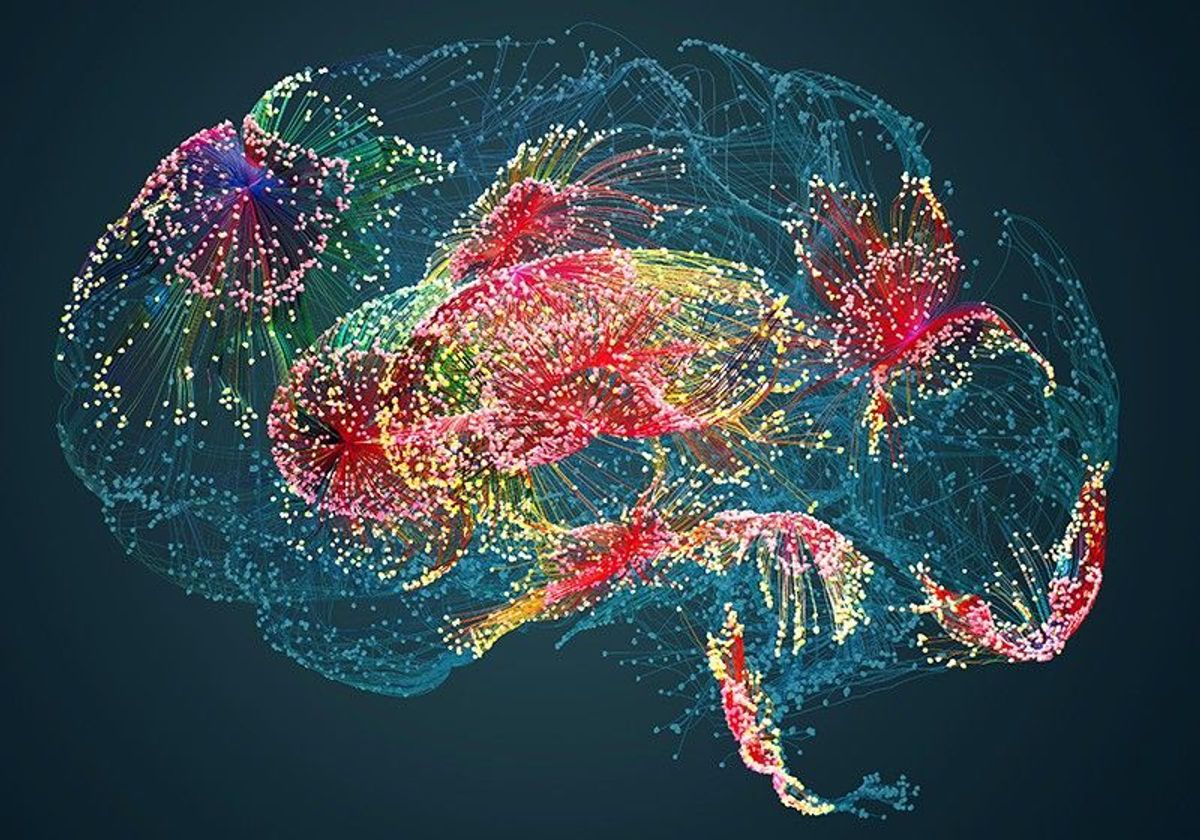
Genes involved in immune system function have atypical expression patterns in the brains of people with some neurological and psychiatric conditions, including autism, according to a new study of thousands of postmortem brain samples.
Of the 1,275 immune genes studied, 765—60 percent—showed elevated or reduced expression in the brains of adults with one of six conditions: autism, schizophrenia, bipolar disorder, depression, Alzheimer’s disease or Parkinson’s disease. The expression patterns varied by condition, suggesting that there are distinct “signatures” for each one, says lead researcher Chunyu Liu, professor of psychiatry and behavioral sciences at Upstate Medical University in Syracuse, New York.
The expression of immune genes could potentially serve as a marker for inflammation, Liu says. Such immune activation—particularly while in utero—has been associated with autism, though the mechanisms are far from clear.
“My impression is the immune system is not really a very minor player in brain disorders,” Liu says. “It is a major player.”
It’s impossible to discern from this study whether immune activation played a role in contributing to any condition or whether the condition itself led to altered immune activation, says Christopher Coe, professor emeritus of biopsychology at the University of Wisconsin-Madison, who was not involved in the work.
“A study of the postmortem brain is informative,” Coe says. “But not definitive.”
See “Excess of Immune Cells Found in Brains of People with Autism”
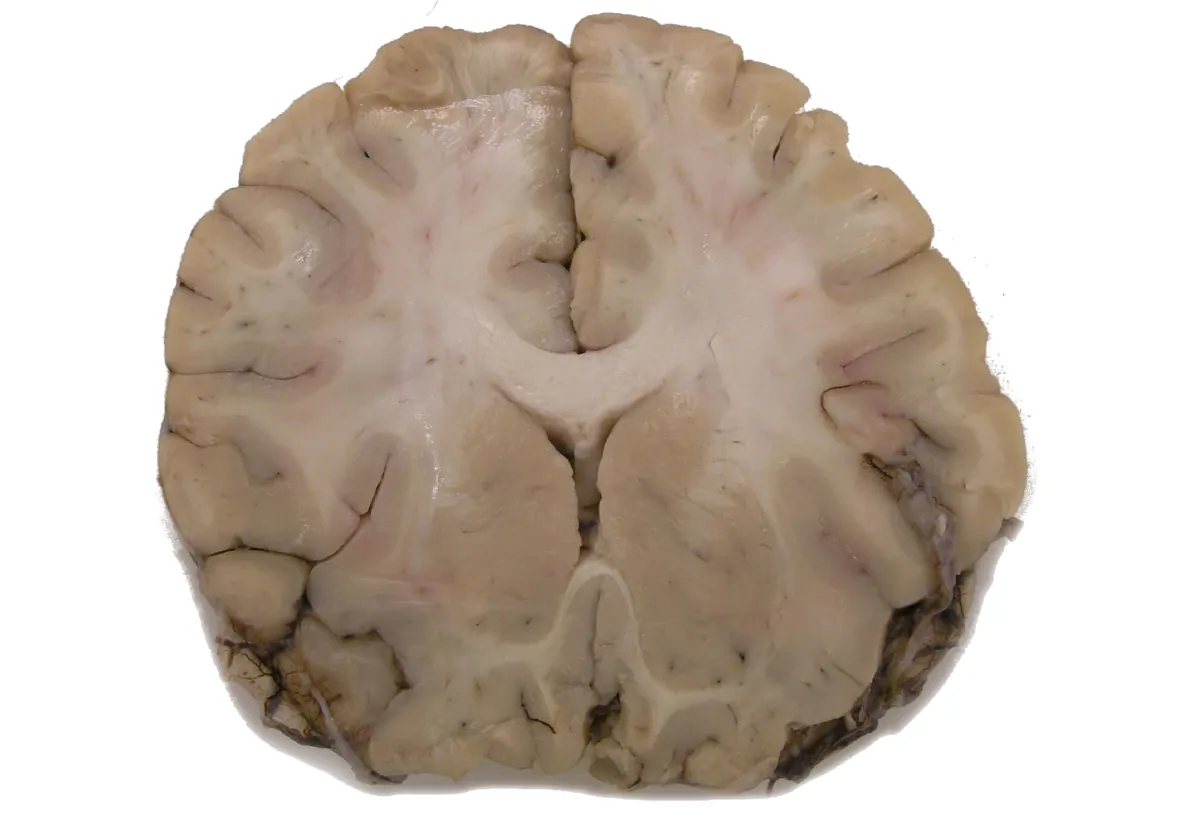
Liu and his team analyzed the expression levels of 1,275 immune genes in 2,467 postmortem brain samples, including 103 from autistic people and 1,178 from controls. The data came from two transcriptomics databases—ArrayExpress and the Gene Expression Omnibus—and other previously published studies.
Brains from autistic people had, on average, 275 genes with expression levels that differed from those of controls; brains from people with Alzheimer’s disease had 638 differentially expressed genes, followed by those with schizophrenia (220), Parkinson’s (97), bipolar disorder (58) and depression (27).
Autistic men’s expression levels varied more than those of autistic women, whereas the brains of women with depression showed more variation than those of men with depression. The other four conditions showed no sex differences.
The autism-related expression pattern more closely resembled those of the neurological conditions—Alzheimer’s and Parkinson’s—than the other psychiatric ones. Neurological conditions, by definition, must have a known physical signature in the brain, such as Parkinson’s characteristic loss of dopaminergic neurons. Researchers have not found such a signature for autism.
“This [similarity] just provides some kind of additional direction we should look into,” Liu says. “Maybe one day we will understand the pathology better.”
The findings were published in Molecular Psychiatry in November.
See “Genetic Underpinnings of Brain Activity May Differ in Autism”
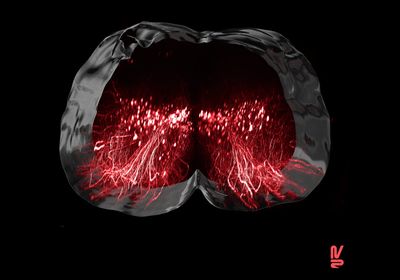
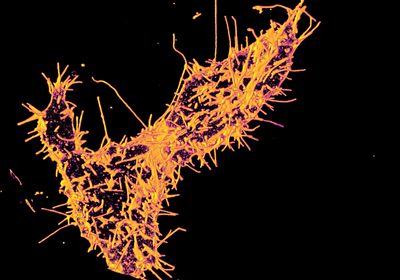
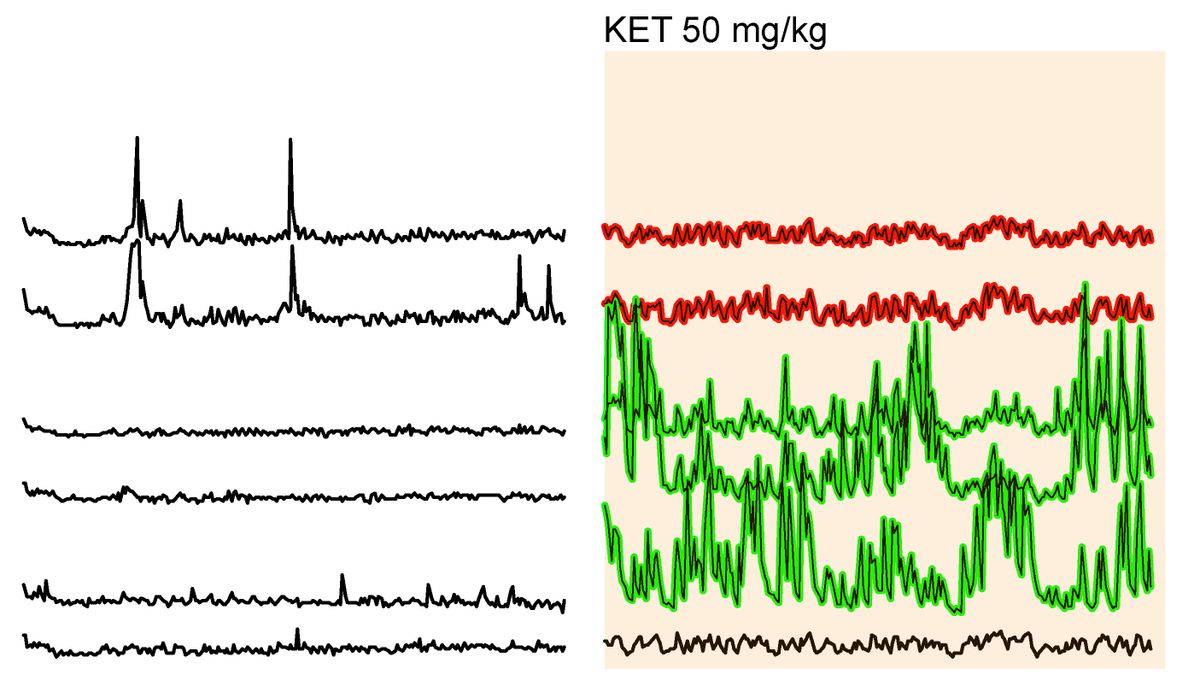
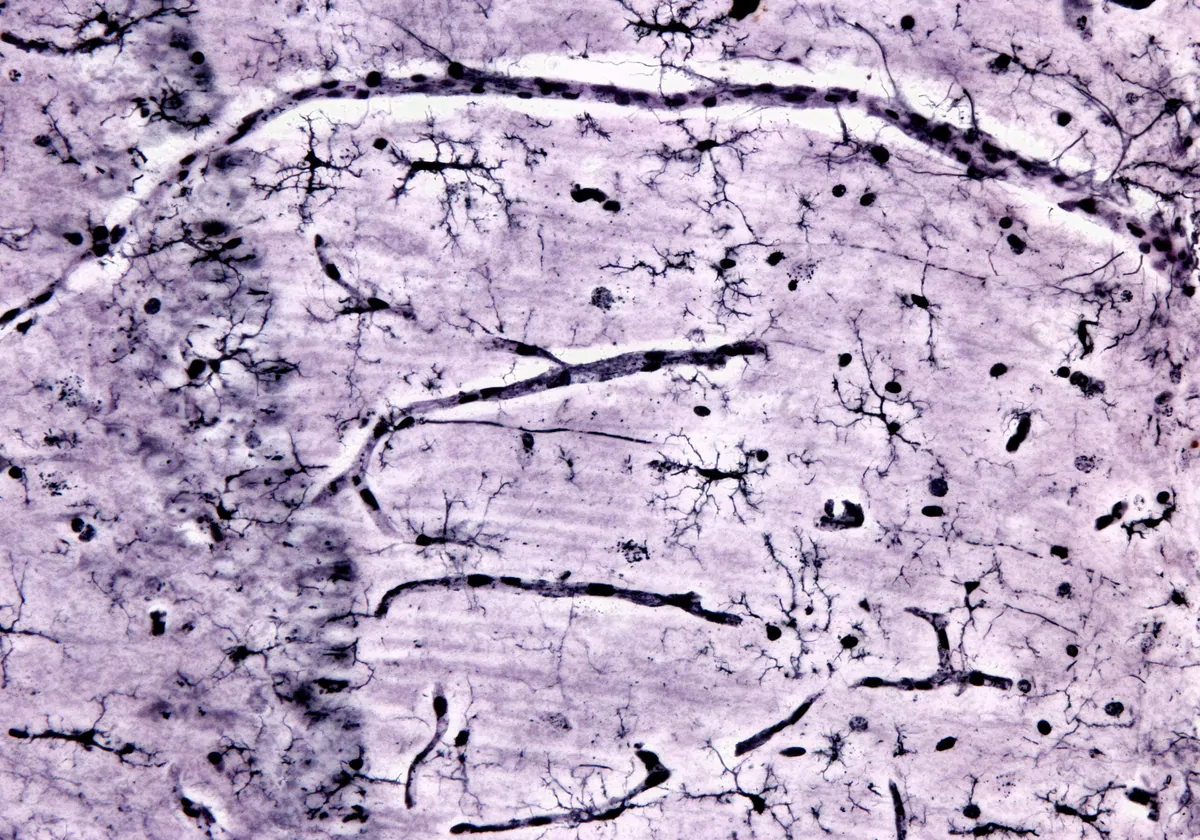
Two genes, CRH and TAC1, are the most commonly altered among the conditions: CRH is downregulated in all of the conditions but Parkinson’s, and TAC1 is downregulated in all but depression. Both genes affect the activation of microglia, the brain’s immune cells.
Atypical microglial activation may be “derailing normal neurogenesis and synaptogenesis,” Coe says, disrupting neuronal activity similarly across the conditions.
Genes involved in astrocyte and synapse function are similarly expressed in people with autism, schizophrenia or bipolar disorder, a 2018 study of postmortem brain tissue found. But microglial genes are overexpressed in autism alone, that study found.
People with more intensely upregulated immune genes could have a “neuroinflammatory condition,” says Michael Benros, professor and head of research on biological and precision psychiatry at the University of Copenhagen in Denmark, who was not involved in the work.
“It could be interesting to try to identify these potential subgroups and of course provide them more specific treatment,” Benros says.
Most of the expression changes observed in the brain tissue samples did not appear in datasets of gene expression patterns in blood samples from people with the same conditions, the study shows. This “somewhat surprising” finding indicates the importance of studying brain tissue, says Cynthia Schumann, professor of psychiatry and behavioral sciences at the University of California Davis MIND Institute, who was not involved in the study.
“If you want to know about the brain, you have to look at the brain itself,” Schumann says.
Liu and his team are creating cellular models to better understand whether inflammation is among the factors that contribute to the development of brain conditions.